
Welcome to the Cardiac Arrest Information Hub of Best Cardiac Hospitals, your trusted source for understanding one of the most urgent and life-threatening medical emergencies. A cardiac arrest occurs when the heart suddenly stops beating effectively, disrupting blood flow to the brain and other vital organs. Unlike a heart attack, which is caused by a blockage in the arteries, cardiac arrest is primarily an electrical issue within the heart. It can happen without warning and requires immediate medical attention to prevent fatal outcomes.
Cardiac Arrest is a sudden and life-threatening event where the heart abruptly stops pumping blood, halting circulation to the brain, lungs, and other essential organs. This condition, if not treated within minutes, can lead to death or irreversible damage. Cardiac arrest is distinct from a heart attack, though the two are often confused. While a heart attack occurs due to blocked blood flow in the coronary arteries, cardiac arrest stems from an electrical malfunction in the heart, disrupting its normal rhythm.
This electrical disruption, often caused by arrhythmias like ventricular fibrillation, results in the heart’s inability to contract effectively. Common triggers for cardiac arrest include pre-existing heart conditions such as coronary artery disease, cardiomyopathy, or congenital defects, as well as external factors like severe trauma, drug overdose, or extreme electrolyte imbalances. Recognizing symptoms such as sudden collapse, loss of consciousness, and absence of a pulse is critical for initiating emergency measures like cardiopulmonary resuscitation (CPR) and defibrillation.
Cardiac arrest occurs when the heart suddenly stops beating, halting blood flow to the brain and other vital organs. It is a life-threatening emergency that requires immediate intervention. While all cardiac arrests are serious, they can occur in different forms depending on the underlying cause and heart's electrical activity. Below are the primary types of cardiac arrest:
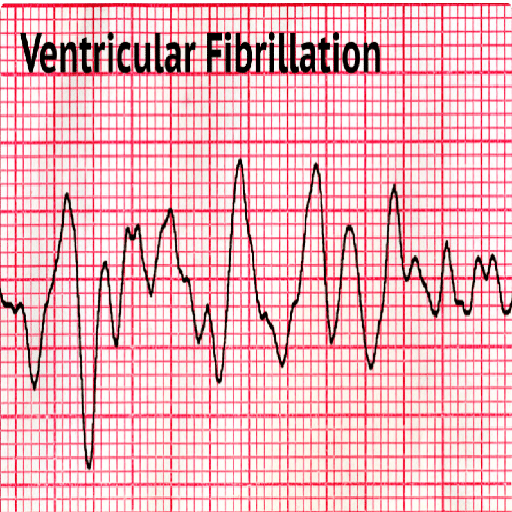
What it is: A chaotic and rapid electrical activity in the ventricles (the heart's lower chambers), causing the heart to quiver instead of pumping blood effectively.
Why it's dangerous: It is the most common cause of cardiac arrest and can lead to sudden death without immediate defibrillation.
Treatment: VF is reversible with rapid defibrillation using an automated external defibrillator (AED) or advanced cardiac life support (ACLS).
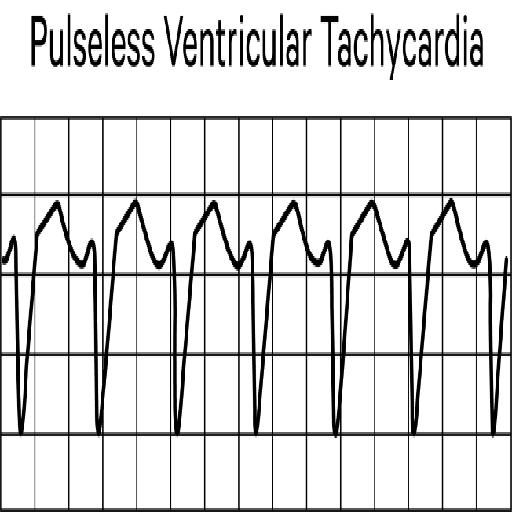
What it is: A fast and abnormal heart rhythm originating in the ventricles, preventing the heart from pumping blood.
Why it's dangerous: The rapid rhythm can lead to loss of pulse and blood circulation, progressing to cardiac arrest.
Treatment: Requires immediate defibrillation and possibly antiarrhythmic medications to restore a normal heart rhythm.
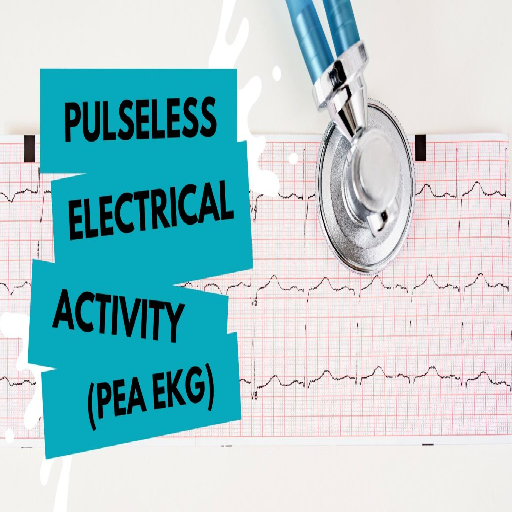
What it is: The heart's electrical system appears to work on monitoring (electrical activity is seen on an ECG), but the heart muscles fail to contract effectively, resulting in no pulse or blood flow.
Why it's dangerous: Often caused by severe underlying conditions such as severe blood loss, electrolyte imbalances, or hypoxia.
Treatment: Defibrillation is not effective. Instead, CPR and treatment of the underlying cause are critical.
What it is: A broad term for any abrupt and unexpected cessation of heart activity, often due to ventricular fibrillation or other electrical disturbances.
Why it's dangerous: It occurs without warning, often in seemingly healthy individuals.
Treatment: Immediate CPR and defibrillation can significantly increase survival chances.

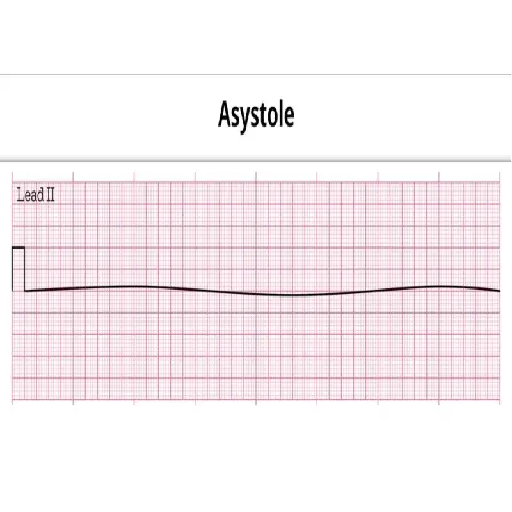
What it is: A total absence of electrical activity in the heart, resulting in no contractions and no blood flow.
Why it's dangerous: It is the final stage of cardiac arrest and has a poor prognosis without immediate intervention.
Treatment: Requires CPR, advanced life support, and addressing reversible causes. Defibrillation is not indicated for asystole.
Cardiac arrest occurs due to a sudden failure in the heart's electrical system, disrupting its ability to pump blood effectively. This malfunction is typically triggered by irregular heart rhythms, or arrhythmias, and can result from a variety of underlying conditions and factors. Understanding these causes is crucial for prevention and management. Below are the most common causes:
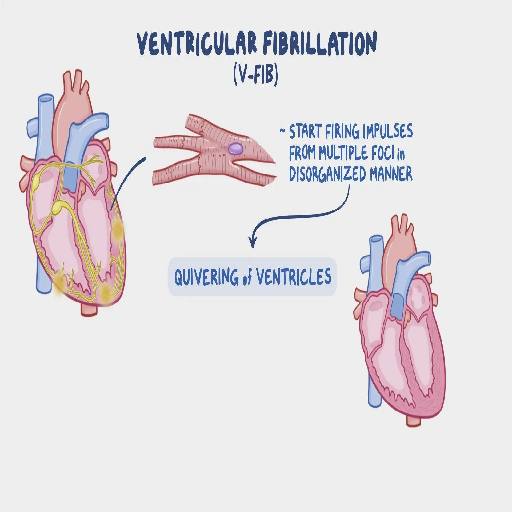
This is the leading cause of cardiac arrest. Ventricular fibrillation involves a rapid, chaotic, and uncoordinated electrical activity in the heart’s lower chambers (ventricles), rendering the heart unable to pump blood efficiently. VF is often triggered by conditions like coronary artery disease or severe heart injury. Without immediate intervention, VF quickly leads to death.
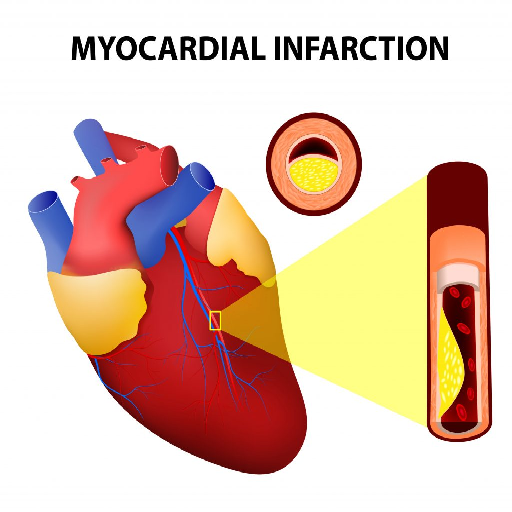
A heart attack, caused by a blockage in the coronary arteries, can damage the heart muscle or its electrical pathways, triggering life-threatening arrhythmias. Approximately half of cardiac arrests occur in individuals who are experiencing or have recently experienced a heart attack.
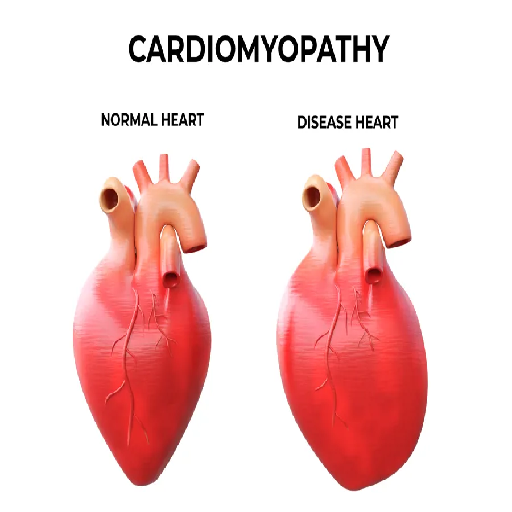
Cardiomyopathy is a condition characterized by structural and functional abnormalities in the heart muscle, which impair the heart’s ability to pump blood effectively and maintain a regular rhythm. The term encompasses several types of heart muscle disorders, each with distinct causes and effects on the heart's function. These abnormalities increase the risk of arrhythmias, heart failure, and in severe cases, cardiac arrest.
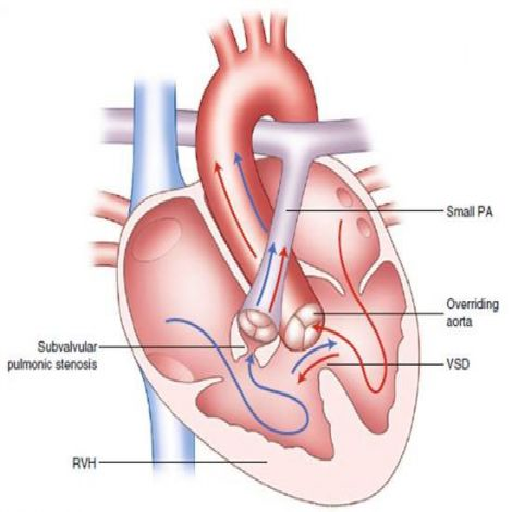
Structural abnormalities in the heart present at birth can disrupt normal blood flow and electrical signaling, making individuals more prone to cardiac arrest. These defects may remain undiagnosed until a serious event occurs.
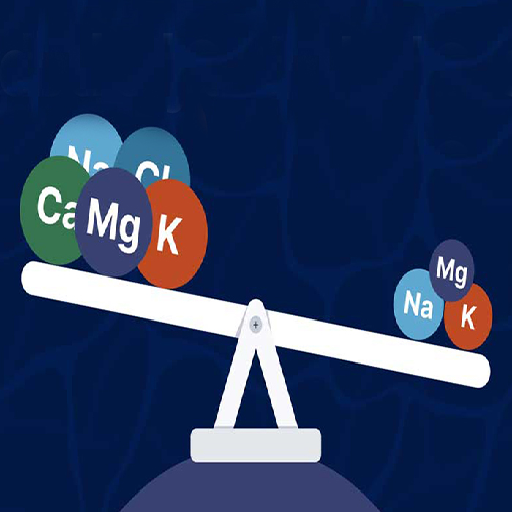
Imbalances in essential minerals like potassium, calcium, and magnesium are critical contributors to the heart’s electrical stability. Extreme deficiencies or excesses can lead to arrhythmias and cardiac arrest.
The misuse of drugs such as cocaine or amphetamines, or an overdose of certain medications, can cause toxic effects on the heart, including arrhythmias that lead to cardiac arrest.
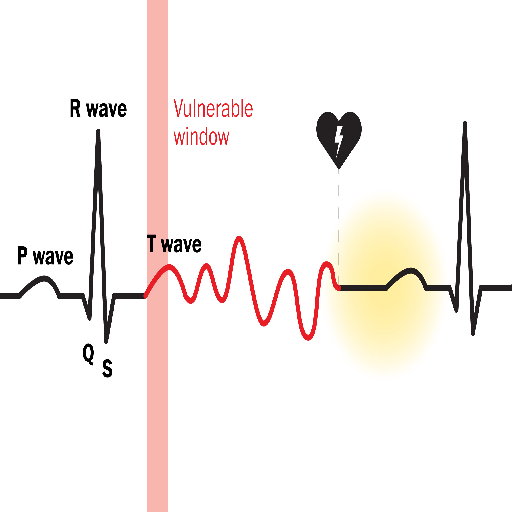
This rare cause involves a sudden, blunt impact to the chest during a specific moment in the heart’s cycle, leading to cardiac arrest. It is most commonly seen in young athletes during sports.
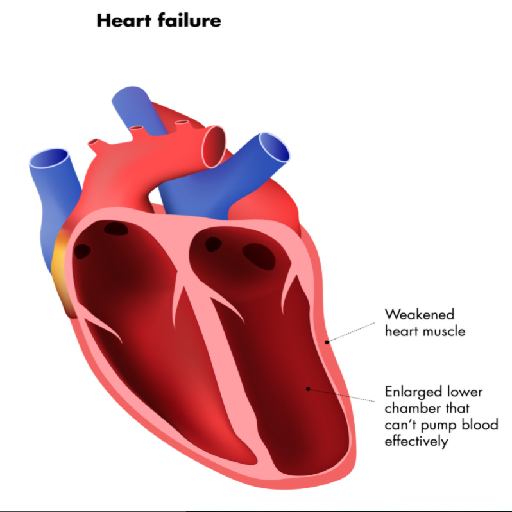
When the heart’s ability to pump blood is significantly compromised, the risk of arrhythmias and cardiac arrest increases. Cardiac arrest is often unpredictable, but many of its underlying causes are linked to chronic heart conditions or lifestyle factors. Regular health check-ups, managing pre-existing conditions, and adopting a heart-healthy lifestyle can significantly lower the risk of cardiac arrest. Immediate recognition of symptoms and prompt treatment are vital to survival.
Cardiac arrest often occurs suddenly and without warning. However, some people experience symptoms in the moments or hours before it happens. These include:

The most obvious and immediate sign.

The person becomes unresponsive.
The heart has stopped pumping blood.

The person is not breathing or is gasping for air.
Treatment focuses on restoring normal heart rhythm, addressing the underlying cause, and preventing future episodes. Here are the main interventions:
While not all cases are preventable, you can significantly reduce your risk with proactive measures:

Eat a balanced diet low in sodium, saturated fats, and trans fats.

Smoking damages blood vessels and increases arrhythmia risk.

Keep blood pressure, cholesterol, and diabetes under control.

If cardiac conditions run in your family, talk to your doctor about screening.
Cardiac arrest is one of the most critical and life-threatening medical emergencies, requiring immediate attention to prevent fatal outcomes. Every second counts, as the heart's sudden cessation of function impacts the oxygen supply to vital organs, especially the brain. However, with the right knowledge and timely intervention, countless lives can be saved. Recognizing the warning signs, such as sudden collapse, absence of a pulse, or irregular breathing, is crucial for initiating life-saving measures like CPR or defibrillation promptly.