
Welcome to the Angina Information Hub of Best Cardiac Hospitals, your trusted resource for understanding this common yet often misunderstood condition. Angina is more than just chest pain; it is a critical warning sign from your heart, indicating that it is not receiving enough oxygen-rich blood. This guide is designed to provide you with clear and compassionate insights into the symptoms, causes, and treatment options for angina. Whether you are newly diagnosed or experiencing unexplained chest discomfort, our goal is to empower you with the knowledge needed to take control of your heart health.
Through this hub, we aim to encourage proactive care and help you make informed decisions about your cardiovascular well-being. Angina is not just a condition to manage—it’s a signal that action is needed to prevent further complications, such as heart attacks. By connecting you with world-class resources, advanced diagnostic tools, and expert care at leading cardiac hospitals, this guide ensures you have access to the support you need. Together, we can work toward improving heart health and enhancing your quality of life.
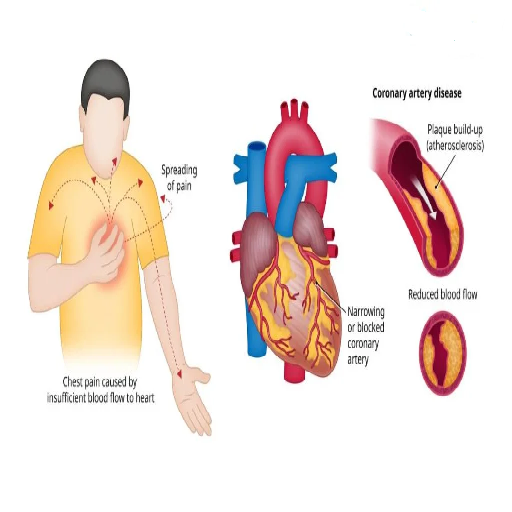
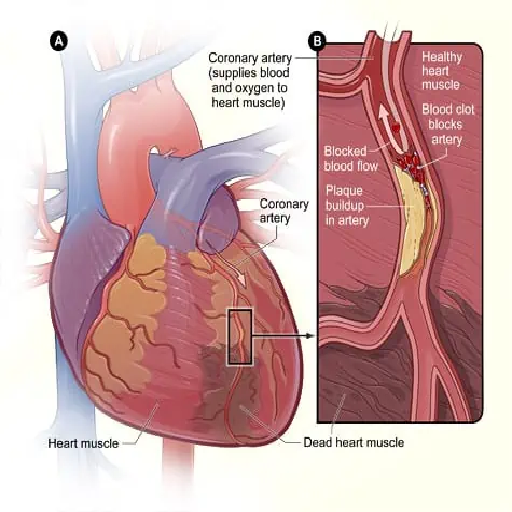
Angina is a medical condition characterized by chest pain or discomfort resulting from reduced blood flow to the heart muscle. Think of your heart as a tirelessly working engine that requires a constant supply of oxygen-rich blood to function efficiently. When this supply is compromised—often due to narrowed or blocked coronary arteries—the heart experiences stress, and angina becomes its warning signal. This discomfort may feel like pressure, heaviness, or a squeezing sensation in the chest and can sometimes extend to the arms, neck, jaw, or back.
Though angina itself is not a disease, it is a crucial symptom pointing to underlying heart conditions, most commonly coronary artery disease (CAD). It can be triggered by physical activity, emotional stress, or even a heavy meal, as these situations increase the heart's demand for oxygen. Angina can be classified into two main types: stable angina, which occurs predictably during exertion, and unstable angina, which can happen unexpectedly and signals a more serious, immediate risk of heart attack. Understanding angina and its triggers is essential for early diagnosis and treatment, helping to prevent more severe complications and improve overall heart health.
Angina presents differently across individuals, and its types provide critical clues about the underlying causes and risks. Each type of angina has unique characteristics, triggers, and implications for heart health. Here's an in-depth look at these distinct forms:
What It Feels Like: A tightness, pressure, or heavy sensation in the chest that may also radiate to the shoulders, arms, or jaw.
When It Occurs: Typically during physical activity or emotional stress, and it subsides with rest or the use of nitroglycerin.
Why It Happens: Stable angina results from partially narrowed coronary arteries that cannot supply enough oxygen-rich blood when the heart's demand increases.
Management: Lifestyle changes, medications like beta-blockers or calcium channel blockers, and, in some cases, surgical interventions can help control symptoms and improve quality of life.
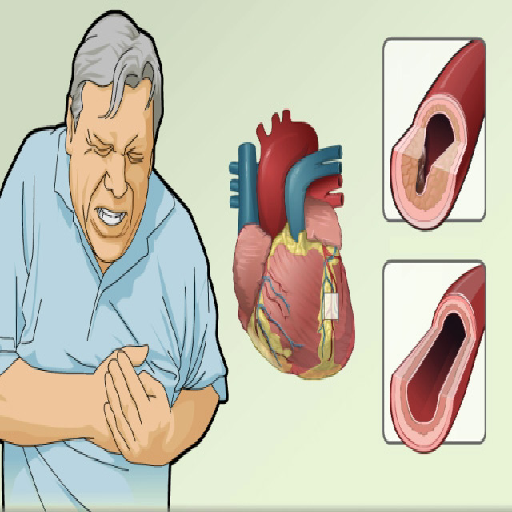
What It Feels Like: A sudden and severe chest pain that often occurs without clear triggers. It may persist longer and feel more intense compared to stable angina.
When It Occurs: It can happen at rest or with minimal exertion, and symptoms do not improve with rest or typical angina medications.
Why It Happens: Caused by blood clots or plaque ruptures that partially or completely block blood flow in the coronary arteries.
Important: Unstable angina is a medical emergency and requires immediate medical attention to prevent a heart attack or further complications.
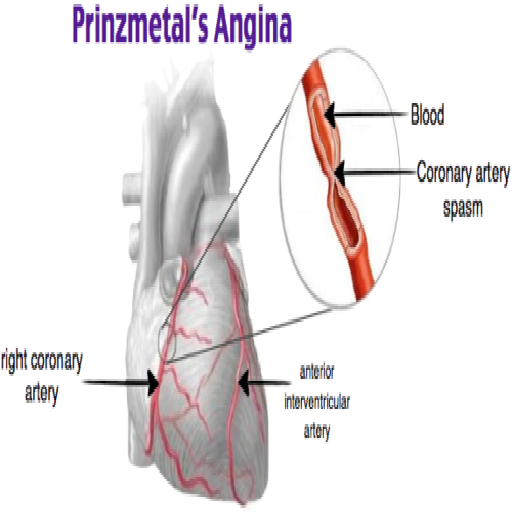
What It Feels Like: Severe chest pain that usually occurs at rest, often during the early morning hours or late at night. The pain can be intense but typically resolves with medication.
Why It Happens: It results from spasms in the coronary arteries, which temporarily reduce blood flow to the heart. These spasms may be triggered by cold exposure, stress, smoking, or certain medications.
Management: Treatment involves medications like calcium channel blockers or nitrates to prevent and manage spasms, along with lifestyle adjustments to minimize triggers.
What It Feels Like: Persistent and diffuse chest pain that is not always relieved by rest or standard angina treatments.
Why It Happens: Unlike other types, microvascular angina is linked to abnormalities in the tiny blood vessels of the heart, rather than blockages in the major arteries.
Management: This type is often treated with medications to improve blood vessel function, such as ACE inhibitors, and strategies to address contributing factors like high blood pressure or stress.
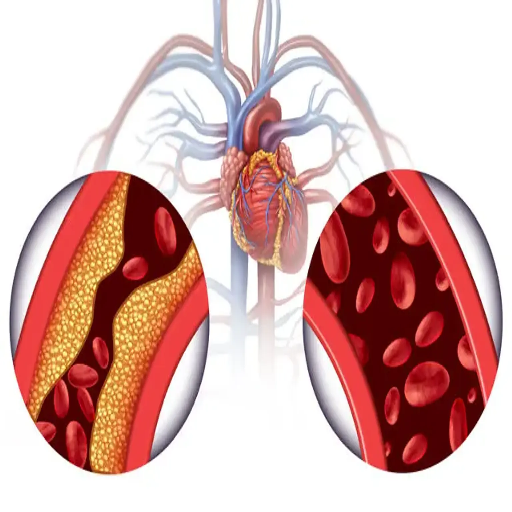
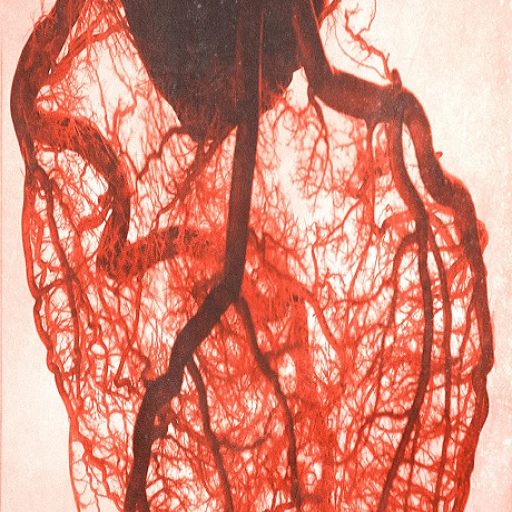
Angina occurs when your heart muscle does not receive enough oxygen-rich blood to meet its needs. This imbalance typically arises from reduced blood flow to the heart, which can be caused by several underlying factors:

The most common cause of angina, CAD, results from the buildup of plaque (atherosclerosis) in the coronary arteries. This narrowing or blockage reduces blood flow, particularly during physical activity or stress, when the heart's demand for oxygen increases.
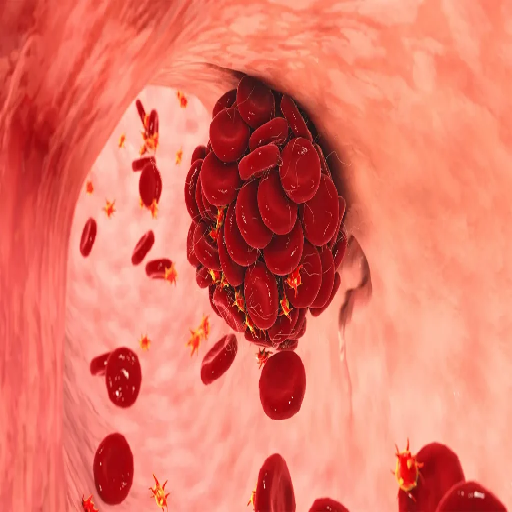
A clot within a coronary artery can partially or completely block blood flow, triggering angina symptoms. These clots often form on the surface of ruptured plaques.
Also known as vasospasms, these sudden, temporary constrictions of the coronary arteries reduce blood flow and can cause angina, even without plaque buildup. Spasms may be triggered by smoking, stress, or exposure to cold temperatures.
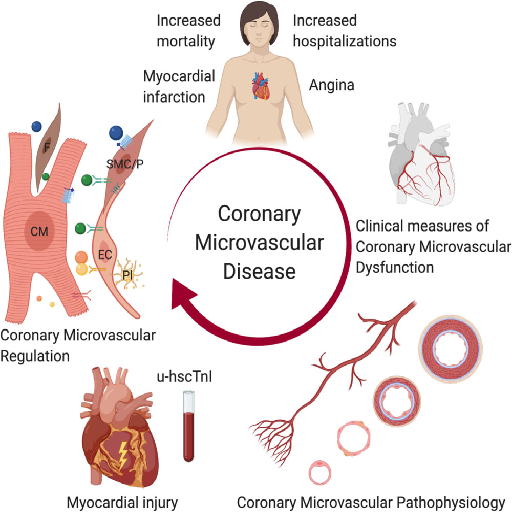
Problems with the smaller blood vessels in the heart (microvasculature) can limit blood flow, leading to a specific type of angina called microvascular angina.

A reduced number of red blood cells can decrease the oxygen-carrying capacity of the blood, limiting the heart's oxygen supply and causing symptoms similar to angina.
Heart diseases often manifest differently in individuals. Below are the most commonly observed symptoms:

Pressure, squeezing, or fullness in the chest.

A feeling of not getting enough air.
Accompanied by sweating in some cases.

Discomfort may spread to the arms, neck, jaw, shoulders, or back.

Unusual tiredness, even during mild activities, may indicate heart strain.
The treatment of angina focuses on managing symptoms, improving blood flow to the heart, and reducing the risk of future complications like heart attacks. A comprehensive approach often includes lifestyle modifications, medications, and in some cases, medical procedures or surgeries tailored to the severity of the condition.
Lifestyle adjustments are foundational in managing angina and promoting heart health:
Medications are often prescribed to manage symptoms, improve blood flow, and prevent complications:
For more severe cases or when medications and lifestyle changes are not sufficient, medical interventions may be necessary:
For individuals recovering from surgeries or dealing with chronic angina, a structured cardiac rehabilitation program can help improve heart health through supervised exercise, dietary counseling, and emotional support.
Effective angina management requires a partnership between the patient and healthcare providers. Regular follow-ups, adherence to treatment plans, and awareness of symptoms can help ensure better outcomes and prevent serious complications.
Prevention is about reducing your risk factors and maintaining a healthy lifestyle:

Limit saturated fats, trans fats, and salt.

If you smoke, seek support to quit.

Learn relaxation techniques to handle stress better.

Aim for at least 150 minutes of moderate exercise weekly.

Keep your blood pressure, cholesterol, and blood sugar in check.
Angina can be a challenging condition to navigate, but with the right knowledge, lifestyle changes, and medical support, it is possible to live a healthy and active life. Your heart is not just an organ—it’s the essence of your vitality, the pulse of your well-being. Listening to your heart’s signals, addressing symptoms early, and taking preventive steps can make a world of difference in ensuring your overall health.
Take charge of your cardiac health today. Whether it’s through adopting a heart-friendly diet, incorporating regular exercise, managing stress, or seeking the right medical treatment, every small action counts toward a healthier tomorrow. Remember, taking care of your heart is an investment in a longer, more fulfilling life.