


Welcome to the Diseases section of Best Cardiac Hospitals, where we delve into the wide array of heart-related conditions treated at leading cardiac care centers. From common ailments such as hypertension and coronary artery disease to complex conditions like arrhythmias and congenital heart defects, these hospitals specialize in managing a diverse range of cardiovascular issues. By understanding the symptoms, underlying causes, and risk factors associated with these diseases, patients and their families can make informed decisions about their healthcare journey. Top cardiac hospitals employ cutting-edge diagnostic technologies, such as echocardiography, angiography, and cardiac MRIs, to ensure accurate assessments and personalized treatment plans.
These hospitals also excel in offering advanced treatment options, ranging from medication management and lifestyle interventions to minimally invasive surgeries and heart transplants. Preventive care is a cornerstone of their approach, empowering individuals with strategies to maintain heart health through proper diet, regular exercise, and stress management. Whether addressing acute emergencies like heart attacks or providing long-term care for chronic conditions, top cardiac hospitals are committed to improving quality of life and promoting cardiovascular wellness for all.
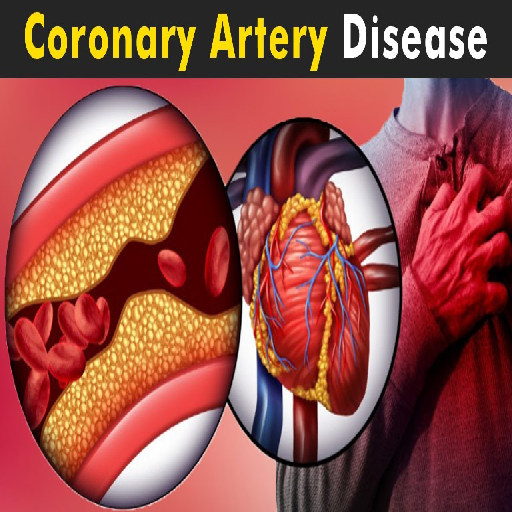
Broad Range of Conditions: Heart diseases, also known as cardiovascular diseases (CVDs), include conditions such as coronary artery disease (blockages in arteries), heart failure (weakened heart pumping ability), arrhythmias (irregular heartbeats), and congenital heart defects (structural issues present at birth).
Global Health Impact: CVDs are the leading cause of death worldwide, with millions of people affected annually. They contribute significantly to the global healthcare burden and are often linked to lifestyle factors and genetic predispositions.
Prevention is Key: Many heart diseases can be prevented by adopting healthier habits, such as maintaining a balanced diet low in saturated fats and sugars, exercising regularly, avoiding tobacco, and managing stress levels effectively.
Importance of Early Detection and Care: Timely medical attention, including routine check-ups, diagnostic tests like ECGs and stress tests, and personalized treatment plans, can greatly enhance survival rates. Advanced interventions, such as stent placement, bypass surgery, and cardiac rehabilitation programs, also play a crucial role in managing these conditions.
Heart diseases develop due to a combination of modifiable and non-modifiable factors:
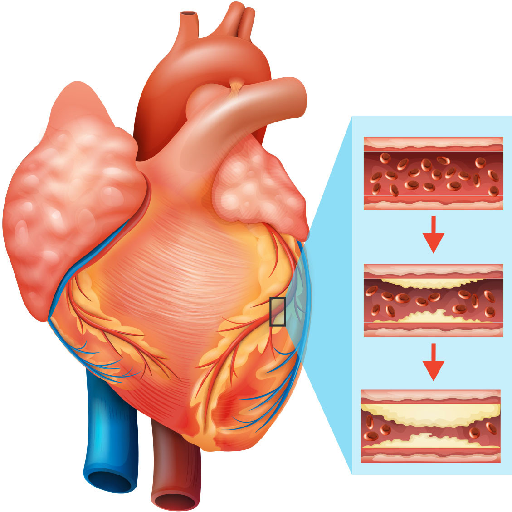
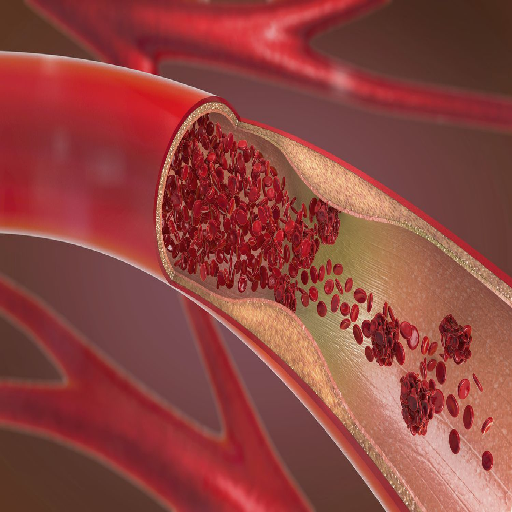
Unhealthy Diet: A diet rich in saturated fats, trans fats, and cholesterol can significantly increase the risk of cardiovascular diseases by promoting plaque buildup in arteries, leading to conditions like atherosclerosis. Additionally, excessive consumption of sugary foods and beverages contributes to obesity and increases the likelihood of developing type 2 diabetes and hypertension. Eating insufficient fruits, vegetables, whole grains, and healthy fats deprives the body of essential nutrients, compounding these risks.
Lack of Physical Activity: A sedentary lifestyle weakens the cardiovascular system over time. Regular physical activity helps maintain a healthy weight, improves blood circulation, and keeps the heart muscles strong. Lack of exercise increases the likelihood of obesity, type 2 diabetes, high blood pressure, and elevated cholesterol levels—all of which are significant contributors to heart disease.
Smoking and Alcohol: Smoking damages blood vessels, reduces oxygen supply, and accelerates the buildup of plaque in arteries. It also raises blood pressure and heart rate, putting undue stress on the heart. Similarly, excessive alcohol consumption weakens the heart muscle, leads to irregular heart rhythms, and raises the risk of high blood pressure, obesity, and stroke. Together, these habits are highly detrimental to cardiovascular health.
Obesity: Obesity is a critical risk factor for a host of health issues, including heart disease, stroke, diabetes, and hypertension. It leads to increased fat deposition around major organs, higher cholesterol levels, and a greater workload on the heart. Obesity also exacerbates inflammatory responses in the body, further complicating cardiovascular health.
Stress: Chronic stress triggers the release of stress hormones like cortisol and adrenaline, which can elevate blood pressure, heart rate, and cholesterol levels. Stress also encourages unhealthy behaviors such as overeating, smoking, drinking alcohol, and neglecting physical activity. Over time, these behaviors compound to significantly increase the risk of cardiovascular problems.
Age: The risk of heart disease increases as people age due to physiological changes in the cardiovascular system. In men, the risk tends to rise significantly after the age of 45, while for women, the risk increases after 55, often linked to hormonal changes following menopause. Aging leads to the stiffening of arteries, a decrease in the elasticity of blood vessels, and an accumulation of fatty deposits, all of which contribute to cardiovascular risk.
Gender: Men generally have a higher risk of developing heart disease earlier in life than women. However, women face a significant increase in risk after menopause due to a drop in protective estrogen levels. While symptoms and risk factors may manifest differently between genders, both men and women need to be vigilant about heart health throughout their lives.
Genetics: A family history of heart disease can significantly increase your likelihood of developing similar conditions. Genetic factors may predispose individuals to high blood pressure, high cholesterol, or structural abnormalities in the heart. If a parent or sibling has experienced a heart attack or been diagnosed with cardiovascular disease, especially at a young age, your risk is substantially higher, emphasizing the need for proactive prevention and regular health screenings.
Below is an extensive overview of the most prevalent heart conditions, categorized for clarity:
Angina Pectoris: Chronic chest pain or discomfort due to reduced blood flow to the heart. It is often triggered by physical activity or stress and serves as a warning sign of underlying coronary artery disease.
Heart Attack (Myocardial Infarction): A complete blockage in the coronary artery that damages heart muscles. Prompt medical intervention is crucial to restore blood flow and minimize permanent heart tissue damage.
Congenital Heart Defects (CHD): Congenital Heart Defects (CHD) are structural abnormalities in the heart present at birth, including issues like holes in the heart walls. These defects can affect blood flow and heart function, requiring specialized medical care.
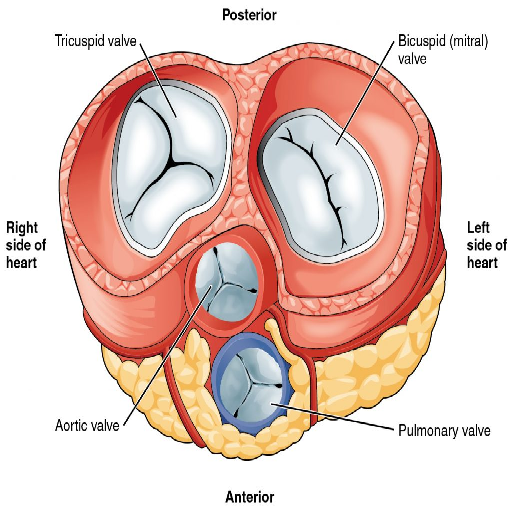
Heart Valve Disorders: Heart Valve Disorders involve malfunctioning valves that disrupt the normal flow of blood through the heart. This can lead to complications such as reduced blood circulation and increased strain on the heart.
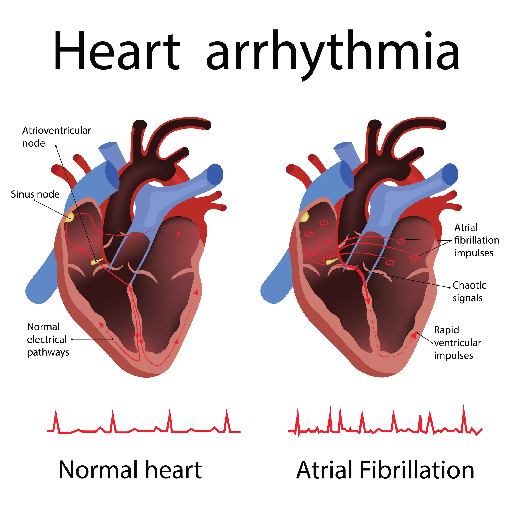
Atrial Fibrillation (AFib): Atrial Fibrillation (AFib) is an irregular and often rapid heart rhythm that can lead to poor blood flow. It increases the risk of stroke, heart failure, and other heart-related complications.
Bradycardia: Bradycardia is a condition characterized by an abnormally slow heart rate, often leading to insufficient blood flow to the body. It can cause fatigue, dizziness, and, in severe cases, heart complications.
Tachycardia: Tachycardia is a condition where the heart beats faster than normal while at rest, potentially reducing its efficiency. It can lead to symptoms like dizziness, shortness of breath, or chest pain, and may require medical attention.
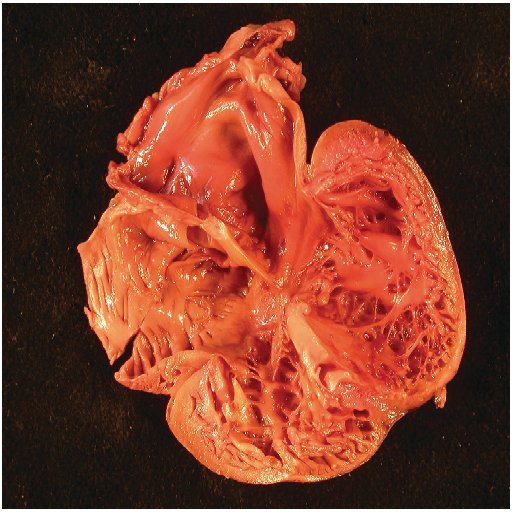
Dilated Cardiomyopathy: Condition where the heart's main pumping chamber becomes enlarged and weakened, reducing its ability to pump blood effectively. This can lead to heart failure and other serious complications.
Hypertrophic Cardiomyopathy: Condition where the heart muscle thickens abnormally, making it harder for the heart to pump blood. It can cause symptoms like chest pain, shortness of breath, and, in some cases, sudden cardiac arrest.
Endocarditis: An infection of the inner lining of the heart chambers and valves, often caused by bacteria entering the bloodstream. It can lead to serious complications, including heart damage, if not treated promptly.
Pericarditis: Inflammation of the pericardium, the thin sac surrounding the heart, often causing chest pain and discomfort. It can result from infections, injury, or autoimmune conditions and may require medical attention.

Definition: Heart failure occurs when the heart cannot pump enough blood to meet the body's oxygen and nutrient needs, leading to fatigue, shortness of breath, and other symptoms.
Underlying Causes: It is often a complication of other heart conditions, such as coronary artery disease, high blood pressure, or previous heart attacks.
Peripheral Artery Disease (PAD): Condition where narrowed arteries reduce blood flow to the limbs, usually the legs. It can cause pain, cramping, and, in severe cases, lead to complications like ulcers or gangrene.
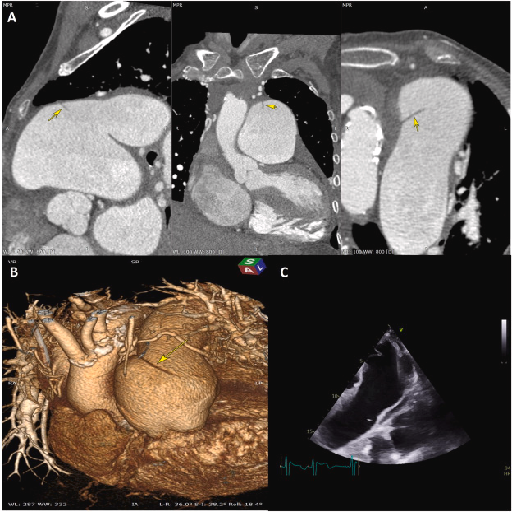
Aneurysm: Bulge or Weakening in the wall of a blood vessel, often in the aorta or brain. If it ruptures, it can lead to life-threatening bleeding or other serious complications.
Pulmonary Hypertension: High blood pressure in the arteries of the lungs, causing strain on the heart. It can lead to symptoms like shortness of breath, fatigue, and chest pain, potentially progressing to heart failure if untreated.
Sudden Cardiac Arrest (SCA): Sudden loss of heart function, breathing, and consciousness, often caused by an electrical disturbance in the heart. It requires immediate medical intervention to prevent fatal outcomes.
Heart diseases develop due to a combination of factors, ranging from physiological conditions to lifestyle choices. Understanding these causes is vital for prevention and early intervention. Below is an expanded explanation of some key contributors to heart disease:
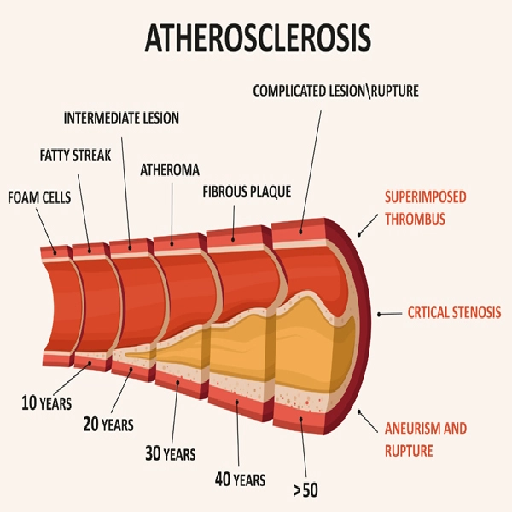
Atherosclerosis is a progressive condition characterized by the buildup of fatty deposits, cholesterol, and other substances in the walls of arteries. Over time, these deposits harden and narrow the arteries, restricting blood flow and increasing the risk of heart attack, stroke, and peripheral vascular disease. Risk factors for atherosclerosis include high cholesterol levels, high blood pressure, smoking, and obesity.
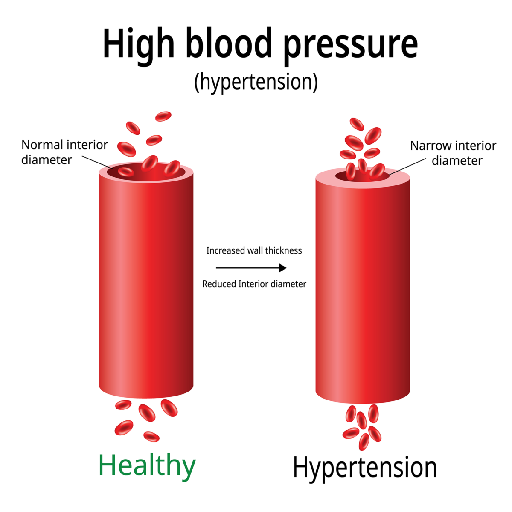
Chronic high blood pressure forces the heart to work harder than normal, causing the heart muscles to thicken and weaken over time. This condition also damages the blood vessels, making them less elastic and more prone to rupture or blockage, leading to complications such as heart failure, aneurysms, or kidney damage.
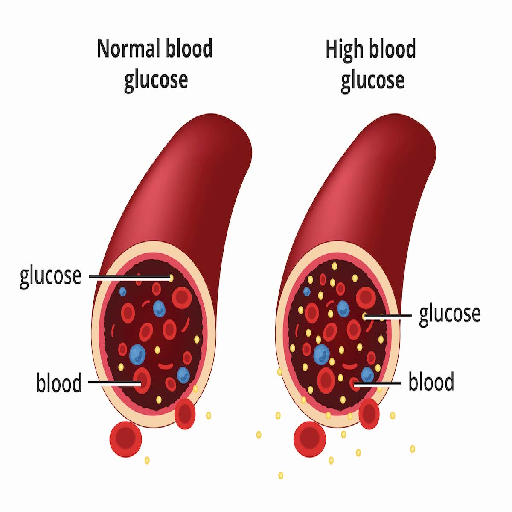
Diabetes is a major contributor to heart disease, as elevated blood sugar levels damage blood vessels and nerves that control the heart. People with diabetes are more likely to develop high blood pressure, high cholesterol, and atherosclerosis, all of which significantly elevate cardiovascular risk.
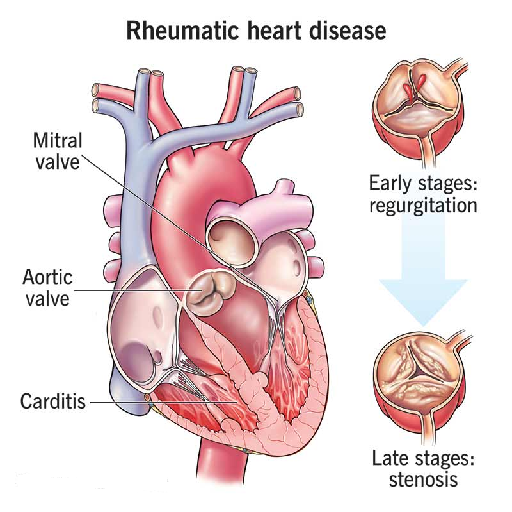
Certain infections, such as rheumatic fever, viral myocarditis, or endocarditis, can cause inflammation of the heart muscle or its surrounding tissues. These conditions can damage the heart valves and impair overall heart function, potentially leading to long-term complications.
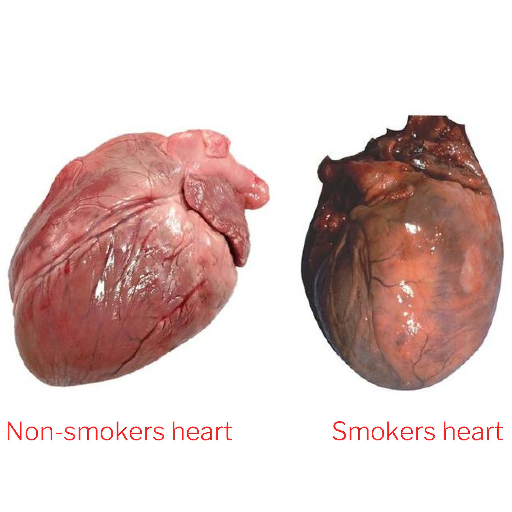
Unhealthy lifestyle habits play a pivotal role in the development and progression of heart disease. Smoking damages the blood vessels, raises blood pressure, and accelerates plaque buildup in the arteries. Poor dietary habits, such as consuming excessive saturated fats, trans fats, and sugar, lead to obesity, high cholesterol, and diabetes. A sedentary lifestyle further exacerbates these risks by contributing to weight gain and poor cardiovascular fitness.
Heart diseases often manifest differently in individuals. Below are the most commonly observed symptoms:

A classic symptom of angina and heart attacks.

Can indicate heart failure or pulmonary hypertension.

May occur with arrhythmias or blood flow issues.

In the legs, ankles, or abdomen due to fluid buildup.

Persistent tiredness, especially during physical activity.

Sweating with chest pain signals danger

Nausea, stomach pain may signal heart.

Irregular heartbeats may signal electrical issues.
Heart disease treatments are highly individualized, depending on the type, severity, and overall health of the patient. The primary goals of treatment are to improve heart function, alleviate symptoms, and prevent further complications. Below is an expanded overview of the comprehensive approaches to managing heart diseases:
Adopting heart-healthy habits is often the first step in treatment.
Medications play a vital role in managing symptoms, reducing risk factors, and treating underlying conditions:
Advanced cases may require surgical intervention to restore or improve heart function:
Innovative technologies and therapies are enhancing treatment outcomes:
Prevention is key to reducing the global burden of cardiovascular diseases. Follow these tips for a heart-healthy life:

Aim for at least 150 minutes of moderate exercise weekly.

Reduces the risk of heart attack by half within a year.

Practice relaxation techniques like meditation or yoga.

Include fruits, vegetables, whole grains, and lean proteins.

Limit alcohol consumption; balance ensures better heart health.
Your heart is the engine of your body—don’t wait for warning signs to take action. Early diagnosis and timely treatment can prevent complications and save lives. If you're experiencing symptoms or have risk factors for heart disease, seeking medical attention promptly can make all the difference. Connect with the world’s leading cardiac hospitals through us for expert care, advanced diagnostics, and personalized treatment plans. Prioritize your heart health today; it’s never too early to take a proactive step towards a healthier future. Contact us now to access the best in cardiac care and support.